Introduction
Urinary tract infections are a serious health problem affecting millions of people each year.

Infections of the urinary tract are the second most common type of infection in the body. Urinary tract infections (UTIs) account for about 8.3 million doctor visits each year. Women are especially prone to UTIs for reasons that are not yet well understood. One woman in five develops a UTI during her
lifetime. UTIs in men are not as common as in women but can be very serious when they do occur.
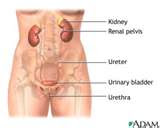
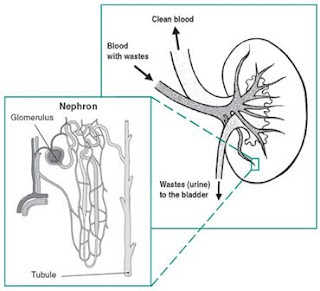
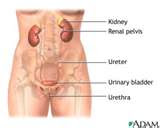
The urinary system consists of the kidneys, ureters, bladder, and urethra. The key elements in the system are the kidneys, a pair of purplish-brown organs located below the ribs toward the middle of the back.
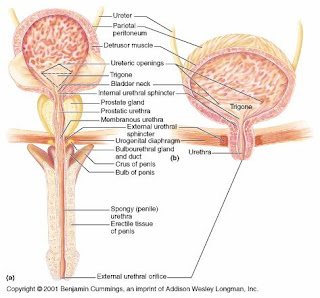
The kidneys remove excess liquid and wastes from the blood in the form of urine, keep a stable balance of salts and other substances in the blood, and produce a hormone that aids the formation of red blood cells. Narrow tubes called ureters carry urine from the kidneys to the bladder, a sack-like organ in the lower abdomen. Urine is stored in the bladder and emptied through the urethra.
The average adult passes about a quart and a half of urine each day. The amount of urine varies, depending on the fluids and foods a person consumes. The volume formed at night is about half that formed in the daytime.
The Urinary System and How It Works
What are the causes of UTI?
Normally, urine is sterile. It is usually free of bacteria, viruses, and fungi but does contain fluids, salts, and waste products. An infection occurs when tiny organisms, usually bacteria from the digestive tract, cling to the opening of the urethra and begin to multiply. The urethra is the tube that carries urine from thebladder to outside the body. Most infections arise from one type of bacteria, Escherichia coli (E. coli), which normally lives in the colon.
In many cases, bacteria first travel to the urethra. When bacteria multiply, an infection can occur. An infection limited to the urethra is called urethritis. If bacteria move to the bladder and multiply, a bladder infection, called cystitis, results. If the infection is not treated promptly, bacteria may then travel further up the ureters to multiply and infect the kidneys. A kidney infection is called pyelonephritis.
Microorganisms called Chlamydia and Mycoplasma may also cause UTIs in both men and women, but these infections tend to remain limited to the urethra and reproductive system. Unlike E. coli, Chlamydia and Mycoplasma may be sexually transmitted, and infections require treatment of both partners.
The urinary system is structured in a way that helps ward off infection. The ureters and bladder normally prevent urine from backing up toward the kidneys, and the flow of urine from the bladder helps wash bacteria out of the body. In men, the prostate gland produces secretions that slow bacterial growth. In both sexes, immune defenses also prevent infection. But despite these safeguards, infections still occur.
Who is at risk?
Some people are more prone to getting a UTI than others. Any abnormality of the urinary tract that obstructs the flow of urine (a kidney stone, for example) sets the stage for an infection. An enlarged prostate gland also can slow the flow of urine, thus raising the risk of infection.
A common source of infection is catheters, or tubes, placed in the urethra and bladder. A person who cannot void or who is unconscious or critically ill often needs a catheter that stays in place for a long time.
Some people, especially the elderly or those with nervous system disorders who lose bladder control, may need a catheter for life. Bacteria on the catheter can infect the bladder, so hospital staff take special care to keep the catheter clean and remove it as soon as possible.

People with diabetes have a higher risk of a UTI because of changes in the immune system. Any other disorder that suppresses the immune system raises the risk of a urinary infection.
UTIs may occur in infants, both boys and girls, who are born with abnormalities of the urinary tract, which sometimes need to be corrected with surgery. UTIs are more rare in boys and young men. In adult women, though, the rate of UTIs gradually increases with age.
Scientists are not sure why women have more urinary infections than men. One factor may be that a woman's urethra is short, allowing bacteria quick access to the bladder.
Also, a woman's urethral opening is near sources of bacteria from the anus and vagina. For many women, sexual intercourse seems to trigger an infection, although the reasons for this linkage are unclear.
According to several studies, women who use a diaphragm are more likely to develop a UTI than women who use other forms of birth control. Recently, researchers found that women whose partners use a condom with spermicidal foam also tend to have growth of E. coli bacteria in the vagina.
=============
RECOMMENDED PRODUCTS:

URINOL is designed to help clear and clean the urinary tract by preventing bacteria from adhering to the wall of the urinary tract, increasing urine flow and inhibiting kidney stone formulation, thereby fighting urinary tract infections and promoting healthy urinary tract and kidney function.
It controls an overactive bladder, stimulates the immune system, and reduces bladder pressure while balancing hormones especially aldosterone.
It also has anti-septic functions than can help the duct of the bladder close. [READ MORE...]
FLUSH 24 IMMUNOL
=============
Recurrent infections
Many women suffer from frequent UTIs. Nearly 20 percent of women who have a UTI will have another, and 30 percent of those will have yet another. Of the last group, 80 percent will have recurrences.
Usually, the latest infection stems from a strain or type of bacteria that is different from the infection before it, indicating a separate infection. Even when several UTIs in a row are due to E. coli, slight differences in the bacteria indicate distinct infections.
Research funded by the National Institutes of Health (NIH) suggests that one factor behind recurrent UTIs may be the ability of bacteria to attach to cells lining the urinary tract.
A recent NIH-funded study found that bacteria formed a protective film on the inner lining of the bladder in mice. If a similar process can be demonstrated in humans, the discovery may lead to new treatments to prevent recurrent UT
Is. Another line of research has indicated that women who are "non-secretors" of certain blood group antigens may be more prone to recurrent UTIs because the cells lining the vagina and urethra may allow bacteria to attach more easily.
Further research will show whether this association is sound and proves useful in identifying women at high risk for UTIs.
Infections in pregnancy
Pregnant women seem no more prone to UTIs than other women. However, when a UTI does occur in a pregnant woman, it is more likely to travel to the kidneys. According to some reports, about 2 to 4 percent of pregnant women develop a urinary infection.
Scientists think that hormonal changes and shifts in the position of the urinary tract during pregnancy make it easier for bacteria to travel up the ureters to the kidneys. For this reason, many doctors recommend periodic testing of urine during pregnancy.
What are the symptoms of UTI?
Not everyone with a UTI has symptoms, but most people get at least some symptoms. These may include a frequent urge to urinate and a painful, burning feeling in the area of the bladder or urethra during urination. It is not unusual to feel bad all over -- tired, shaky, washedout -- and to feel pain even when not urinating.
Often women feel an uncomfortable pressure above the pubic bone, and some men experience a fullness in the rectum. It is common for a person with a urinary infection to complain that, despite the urge to urinate, only a small amount of urine is passed. The urine itself may look milky or cloudy, even reddish if blood is present.
Normally, a UTI does not cause fever if it is in the bladder or urethra. A fever may mean that the infection has reached the kidneys. Other symptoms of a kidney infection include pain in the back or side below the ribs, nausea, or vomiting.
In children, symptoms of a urinary infection may be overlooked or attributed to another disorder. A UTI should be considered when a child or infant seems irritable, is not eating normally, has an unexplained fever that does not go away, has incontinence or loose bowels, or is not thriving.
Unlike adults, children are more likely to have fever and no other symptoms. This can happen to both boys and girls. The child should be seen by a doctor if there are any questions about these symptoms, especially a change in the child's urinary pattern.
How is a UTI diagnosed?
To find out whether you have a UTI, your doctor will test a sample of urine for pus and bacteria. You will be asked to give a "clean catch" urine sample by washing the genital area and collecting a "midstream" sample of urine in a sterile container.
This method of collecting urine helps prevent bacteria around the genital area from getting into the sample and confusing the test results. Usually, the sample is sent to a laboratory, although some doctors' offices are equipped to do the testing.
In the urinalysis test, the urine is examined for white and red blood cells and bacteria. Then the bacteria are grown in a culture and tested against different antibiotics to see which drug best destroys the bacteria. This last step is called a sensitivity test.
Some microbes, like Chlamydia and Mycoplasma, can be detected only with special bacterial cultures. A doctor suspects one of these infections when a person has symptoms of a UTI and pus in the urine, but a standard culture fails to grow any bacteria.
When an infection does not clear up with treatment and is traced to the same strain of bacteria, the doctor may order some tests to determine if your system is normal.
One of these tests is an intravenous pyelogram, which gives x-ray images of the bladder, kidneys, and ureters. An opaque dye visible on x-ray film is injected into a vein, and a series of x-rays is taken. The film shows an outline of the urinary tract, revealing even small changes in the structure of the tract.
If you have recurrent infections, your doctor also may recommend an ultrasound exam, which gives pictures from the echo patterns of soundwaves bounced back from internal organs. Another useful test is cystoscopy. A cystoscope is an instrument made of a hollow tube with several lenses and a light source, which allows the doctor to see inside the bladder from the urethra.
How is UTI treated?
UTIs are treated with antibacterial drugs. The choice of drug and length of treatment depend on the patient's history and the urine tests that identify the offending bacteria. The sensitivity test is especially useful in helping the doctor select the most effective drug.
The drugs most often used to treat routine, uncomplicated UTIs are trimethoprim (Trimpex), trimethoprim/sulfamethoxazole (Bactrim, Septra, Cotrim), amoxicillin (Amoxil, Trimox, Wymox), nitrofurantoin (Macrodantin, Furadantin), and ampicillin (Omnipen, Polycillin, Principen, Totacillin). A class of drugs called quinolones includes four drugs approved in recent years for treating UTI. These drugs include ofloxacin (Floxin), norfloxacin (Noroxin), ciprofloxacin (Cipro), and trovafloxin (Trovan).
Often, a UTI can be cured with 1 or 2 days of treatment if the infection is not complicated by an obstruction or other disorder. Still, many doctors ask their patients to take antibiotics for a week or two to ensure that the infection has been cured.
Single-dose treatment is not recommended for some groups of patients, for example, those who have delayed treatment or have signs of a kidney infection, patients with diabetes or structural abnormalities, or men who have prostate infections.
Longer treatment is also needed by patients with infections caused by Mycoplasma orChlamydia, which are usually treated with tetracycline, trimethoprim/sulfamethoxazole (TMP/SMZ), or doxycycline. A followup urinalysis helps to confirm that the urinary tract is infection-free. It is important to take the full course of treatment because symptoms may disappear before the infection is fully cleared.
Severely ill patients with kidney infections may be hospitalized until they can take fluids and needed drugs on their own. Kidney infections generally require several weeks of antibiotic treatment. Researchers at the University of Washington found that 2-week therapy with TMP/SMZ was as effective as 6 weeks of treatment with the same drug in women with kidney infections that did not involve an obstruction or nervous system disorder. In such cases, kidney infections rarely lead to kidney damage or kidney failure unless they go untreated.
Various drugs are available to relieve the pain of a UTI. A heating pad may also help. Most doctors suggest that drinking plenty of water helps cleanse the urinary tract of bacteria. During treatment, it is best to avoid coffee, alcohol, and spicy foods. And one of the best things a smoker can do for his or her bladder is to quit smoking. Smoking is the major known cause of bladder cancer.
Recurrent infections in women
Women who have had three UTIs are likely to continue having them. Four out of five such women get another within 18 months of the last UTI. Many women have them even more often. A woman who has frequent recurrences (three or more a year) can ask her doctor about one of the following treatment options:
- Take low doses of an antibiotic such as TMP/SMZ or nitrofurantoin daily for 6 months or longer. If taken at bedtime, the drug remains in the bladder longer and may be more effective. NIH-supported research at the University of Washington has shown this therapy to be effective without causing serious side effects.
- Take a single dose of an antibiotic after sexual intercourse.
- Take a short course (1 or 2 days) of antibiotics when symptoms appear.
Dipsticks that change color when an infection is present are now available without a prescription. The strips detect nitrite, which is formed when bacteria change nitrate in the urine to nitrite. The test can detect about 90 percent of UTIs when used with the first morning urine specimen and may be useful for women who have recurrent infections.
Doctors suggest some additional steps that a woman can take on her own to avoid an infection:
- Drink plenty of water every day.
- Urinate when you feel the need; don't resist the urge to urinate.
- Wipe from front to back to prevent bacteria around the anus from entering the vagina or urethra.
- Take showers instead of tub baths.
- Cleanse the genital area before sexual intercourse.
- Avoid using feminine hygiene sprays and scented douches, which may irritate the urethra.
Some doctors suggest drinking cranberry juice.
Infections in pregnancy
A pregnant woman who develops a UTI should be treated promptly to avoid premature delivery of her baby and other risks such as high blood pressure. Some antibiotics are not safe to take during pregnancy. In selecting the best treatments, doctors consider various factors such as the drug's effectiveness, the stage of pregnancy, the mother's health, and potential effects on the fetus.
Complicated infections
Curing infections that stem from a urinary obstruction or other systemic disorders depends on finding and correcting the underlying problem, sometimes with surgery. If the root cause goes untreated, this group of patients is at risk of kidney damage. Also, such infections tend to arise from a wider range of bacteria, and sometimes from more than one type of bacteria at a time.
Infections in men
UTIs in men are often a result of an obstruction -- for example, a urinary stone or enlargedprostate -- or from a medical procedure involving a catheter. The first step is to identify the infecting organism and the drugs to which it is sensitive. Usually, doctors recommend lengthier therapy in men than in women, in part to prevent infections of the prostate gland.
Prostate infections (chronic bacterial prostatitis) are harder to cure because antibiotics are unable to penetrate infected prostate tissue effectively. For this reason, men with prostatitis often need long-term treatment with a carefully selected antibiotic. UTIs in older men are frequently associated with acute bacterial prostatitis, which can have serious consequences if not treated urgently.
Is there a vaccine to prevent recurrent UTIs?
In the future, scientists may develop a vaccine that can prevent UTIs from coming back. Researchers in different studies have found that children and women who tend to get UTIs repeatedly are likely to lack proteins called immunoglobulins, which fight infection. Children and women who do not get UTIs are more likely to have normal levels of immunoglobulins in their genital and urinary tracts.
Early tests indicate that a vaccine helps patients build up their own natural infection-fighting powers. The dead bacteria in the vaccine do not spread like an infection; instead, they prompt the body to produce antibodies that can later fight against live organisms. Researchers are testing injected and oral vaccines to see which works best. Another method being considered for women is to apply the vaccine directly as a suppository in the vagina.
- The urinary tract consists of the kidneys, ureters, bladder, and urethra.
- Some people are at more risk for urinary tract infections (UTIs) than others.
- One woman in five develops a UTI during her lifetime.
- Not everyone with a UTI has symptoms. Common symptoms include a frequent urge to urinate and a painful, burning when urinating.
- Underlying conditions that impair the normal urinary flow can lead to more complicated UTIs.
[Source: National Institutes of Health, National Kidney and Urologic Diseases Information Clearinghouse]